Scroll to:
PREVALENCE OF CARDIOVASCULAR RISK FACTORS AMONG INDIVIDUALS WITH NORMOTENSION, PREHYPERTENSION, AND HYPERTENSION
https://doi.org/10.57256/2949-0715-2025-4-4-31-38
Abstract
Relevance. Hypertension is a leading global health burden and a major risk factor for cardiovascular disease and premature mortality. Prehypertension, particularly in young adults, often goes unrecognized but predicts future hypertension. Both modifiable factors – diet, physical activity, tobacco use, and stress – and non-modifiable factors – age, sex, and family history – affect blood pressure. Early detection is essential for prevention.
Aim. To assess the prevalence of normotension, prehypertension, and hypertension, and their associated risk factors among adults in a tertiary medical institution in Jaipur, India.
Materials and methods. A cross-sectional study was conducted over 6 months among 700 participants aged 18–60 years at Rajasthan University of Health Sciences College of Medical Sciences and Associated Hospitals, Jaipur. Blood pressure was measured according to Ministry of Health and Family Welfare guidelines. Socio-demographic, anthropometric, and lifestyle data were collected. Statistical analysis was performed using SPSS v16, with p < 0.05 considered significant.
Results. Of 700 participants (56 % male; mean age 22.8 ± 6.7 years), 65,0 % were normotensive, 34,9 % prehypertensive, and 0,02 % hypertensive. Prehypertension was more common in males, urban residents, physically inactive individuals, and those with obesity, central obesity, high salt intake, tobacco or alcohol use, or moderate-to-severe stress. Family history of hypertension was more frequent in prehypertensive and hypertensive participants.
Conclusion. Prehypertension is prevalent among young adults and is strongly associated with modifiable lifestyle factors and family history. Early identification and targeted lifestyle interventions are crucial to prevent progression to hypertension and reduce long-term cardiovascular risk.
For citations:
Tyagi A., Kacker S., Saboo N., Kumar M. PREVALENCE OF CARDIOVASCULAR RISK FACTORS AMONG INDIVIDUALS WITH NORMOTENSION, PREHYPERTENSION, AND HYPERTENSION. Baikal Medical Journal. 2025;4(4):31-38. https://doi.org/10.57256/2949-0715-2025-4-4-31-38
Introduction
Blood pressure is a critical physiological parameter representing the force exerted by circulating blood on the arterial walls, which varies during the cardiac cycle. Systolic blood pressure (SBP) is the maximum pressure recorded during ventricular systole and primarily depends on cardiac output and arterial compliance, while diastolic blood pressure (DBP) represents the minimum pressure during diastole and depends on total peripheral resistance [1]. Stiffening of arteries with age results in higher systolic pressure, whereas alterations in vascular diameter and blood viscosity influence diastolic pressure.
According to the Ministry of Health and Family Welfare, adult blood pressure is categorized as normotensive (<120/80 mmHg), prehypertensive (130–139/85–89 mmHg), and hypertensive (≥140/90 mmHg). Prehypertension is considered a precursor state, increasing the risk of progression to overt hypertension if lifestyle interventions are not adopted [2].
Hypertension is a major public health concern worldwide, contributing significantly to cardiovascular morbidity and mortality, including coronary artery disease, stroke, heart failure, and renal complications. Globally, an estimated 1 billion people suffer from elevated blood pressure, accounting for approximately 13,5 % of total premature deaths. In India, the prevalence of hypertension is steadily rising due to urbanization, sedentary lifestyles, dietary changes, and increasing life expectancy [3].
The risk factors for hypertension can be broadly classified into non-modifiable (age, gender, family history) and modifiable factors (obesity, physical inactivity, high salt intake, tobacco and alcohol use, and stress). Modifiable factors play a key role in the transition from normotension to prehypertension and eventually hypertension. Among these, overweight and obesity lead to activation of the renin–angiotensin–aldosterone system (RAAS) and sympathetic overactivity, causing vasoconstriction and sodium retention. Excess salt intake increases extracellular fluid volume and blood pressure, while tobacco use and psychological stress exacerbate vascular reactivity [4].
Prehypertension and hypertension are often asymptomatic, earning the title of «silent killers». Early identification of at-risk individuals through community-based screening and evaluation of associated risk factors is vital to reduce the future burden of cardiovascular disease. Lifestyle modifications, including weight management, increased physical activity, dietary salt reduction, and stress management, have been shown to significantly reduce the risk of progression to hypertension.
Materials and methods
Study Design: this was an observational study conducted to assess the prevalence of normotensive, pre-hypertensive, and hypertensive individuals and their associated risk factors in RUHS college of Medical Sciences and Associated Hospitals, Jaipur.
Study Setting and Population: the study was carried out at Rajasthan University of Health Sciences (RUHS) College of Medical Sciences and Associated Hospitals, Jaipur, involving the working population including medical and paramedical students, teaching staff, non-teaching staff, guards, and laborers aged 18–60 years.
Study Duration: 6 months
Study Universe: 1300 subjects.
Sample Size: 700 subjects.
Calculated using mean and standard deviation formula at 95 % confidence interval and 80 % power, with 10 % dropout rate considered (calculated sample = 696, final = 700).
Inclusion Criteria: age between 18–60 years.
Subjects who provided written consent.
Alcoholic and smokers were included.
Exclusion Criteria:
Pregnant women.
Individuals with chronic illnesses (ischemic heart disease, coronary artery disease, stroke, acute/chronic kidney disease).
Those on anti-hypertensive therapy (diuretics, Angiotensin-converting enzyme (ACE) inhibitors, beta-blockers, calcium channel blockers).
Ethical Considerations: approval obtained from RUHS-CMS Ethics Committee (EC/P-62/2021). Written informed consent was taken from all participants.
Statistical Analysis: data analyzed using SPSS version 16.0 (Chicago, Inc., USA). Normality checked using Shapiro-Wilk test. Mean ± SD calculated for continuous variables. Pearson’s t-test used for categorical comparisons. p-value < 0,05 considered statistically significant.
Results
The present observational study was conducted among 700 participants aged 18–60 years (mean age 22,77 ± 6,67 years) at RUHS College of Medical Sciences and Associated Hospitals, Jaipur. Among these, 395 (56 %) were males and 305 (44 %) were females, with the majority residing in urban areas (62,4 %), followed by semi-urban (17,8 %) and rural (19,7 %) regions. The majority of the participants were unmarried (91 %), and 85 % were college students (table 1).
Table 1: Anthropometric parameter Age, Height, Weight, Body mass index, Waist circumference, Hip circumference and Waist to hip ratio of the study population
SN. | Parameters | Total particiapants (n = 700) mean±SD |
1. | Age (Years) | 22,77 ± 6,7 |
2. | Height (cm) | 166,90±7,6 |
3. | Weight (Kg) | 59,3±11,2 |
4. | BMI (kg/m2) | 21,2 ±3,6 |
5. | SBP (mmHg) | 118,5±8,2 |
6. | DBP (mmHg) | 78,5±6,0 |
7. | Waist circumference | 87,4± 13,3 |
8. | Hip circumference | 94,4± 13,6 |
9. | Waist - to-hip ratio | 0,9±0,002 |
Note: S.D.=standard deviation, mmHg= millimeter of mercury, Cm= centrimeters, Kg= kilogram, SBP= Sytolic blood pressure, DBP= Diastolic blood pressure, BMI= Body mass index,
The baseline characteristics of the study population (n = 700). Participants were predominantly young (mean age 22,8 years) with normal BMI (21,2 kg/m²). Mean SBP (118,5 mmHg) and DBP (78,5 mmHg) were within normal limits, while anthropometric indices (waist circumference 87,4 cm, hip circumference 94,9 cm, WHR 0.9) indicated balanced fat distribution.
Prevalence of Blood Pressure Categories
The distribution of participants according to their blood pressure status, based on Ministry of Health and Family Welfare criteria, is summarized in Fig. 1.
The majority of participants, 65 %, were normotensive. Approximately 34,8 % of participants were pre-hypertensive, indicating a substantial portion at risk for developing hypertension. Only a very small fraction, 0,2 %, were hypertensive, reflecting a low prevalence of hypertension in this population. Overall, the graph highlights that most of the study population had normal blood pressure, while about one-third were at an elevated risk.
Mean SBP: 118,48 ± 8,15 mmHg, Mean DBP: 78,46 ± 5.96 mmHg. A majority of participants (65 %) were normotensive. Pre-hypertension constituted ~ 35 %, indicating a significant at-risk population for future hypertension. Hypertension prevalence (0,02 %) was very low, likely due to the predominantly young population in the study.
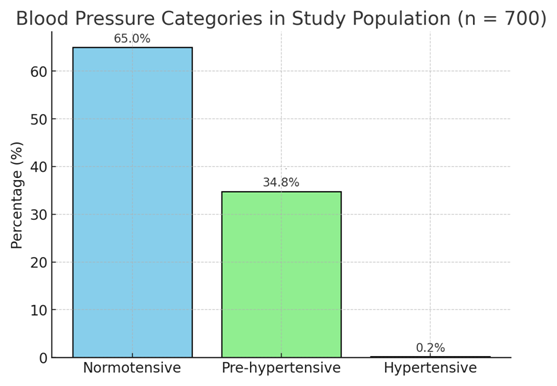
Fig. 1. Illustrates that the distribution of blood pressure categories among 700 participants in the study.
Association of Risk Factors with Blood Pressure Status
Multiple modifiable and non-modifiable risk factors were analyzed to determine their association with pre-hypertension and hypertension.
A. Non-Modifiable risk Factors (table 3):
Age: Pre-hypertension increased with advancing age, though the majority of the sample was 18–22 years (78,4 %).
Gender: Males had a higher proportion of pre-hypertension compared to females.
Residence: Urban residents exhibited higher prevalence of pre-hypertension compared to rural participants, reflecting urban lifestyle and dietary habits.
- Modifiable Lifestyle Factors (table 4):
Physical Activity: 46,2 % of participants were inactive, and this group demonstrated higher pre-hypertension prevalence, highlighting physical inactivity as a significant risk factor.
Obesity (BMI & Waist-to-Hip Ratio): Overweight and obese individuals showed a strong correlation with pre-hypertension. Central obesity (waist-to-hip ratio >0,95 in males and >0,85 in females) was observed in many pre-hypertensive participants.
Stress (Perceived Stress Scale): Moderate to severe stress scores were strongly linked with pre-hypertension. Chronic stress is known to stimulate sympathetic activity, contributing to transient blood pressure elevation.
Tobacco and Alcohol Use: Smokers and alcohol users showed a trend toward higher blood pressure, consistent with nicotine and alcohol-induced vascular effect.
Table 3. Association of Non-Modifiable Risk Factors with Blood Pressure Status
Study Parameters | N | Normal (%) | Pre-Hypertension (%) | Hypertension (%) |
Age Group (Yrs) |
|
|
|
|
18-22 | 549 | 369 (52.7%) | 109 (15.57%) | - |
23-27 | 70 | 58 (8.2%) | 82 (11.71%) | - |
28-32 | 29 | 13 (1.85%) | 15 (2.14%) | - |
33-37 | 5 | 1 (0.14%) | 4 (0.57%) | - |
38-42 | 21 | 6 (0.85%) | 15 (2.14%) | - |
43-47 | 12 | 4 (0.57%) | 8 (1.14%) | 1 (0.14%) |
48-52 | 9 | 4 (0.57%) | 6 (0.85%) | 1 (0.14%) |
53-57 | 2 | - | 2 (0.28%) | - |
58-60 | 3 | - | 2 (0.28%) | - |
23-27 | 70 | 369 (52.7%) | 109 (15.57%) | - |
28-32 | 29 | 58 (8.2%) | 82 (11.71%) | - |
Gender |
|
|
|
|
Male | 395 | 255 (36.4%) | 139 (19.85%) | 1 (0.14%) |
Female | 305 | 203 (29%) | 101 (14.42%) | 1 (0.14%) |
Family History of Hypertension |
|
|
|
|
No | 288 | 174 (24.8%) | 113 (16.1%) | 1 (0.14%) |
Yes | 412 | 257 (36.7%) | 154 (22%) | 1 (0.14%) |
Table 4. Association of Modifiable Risk Factors with Blood Pressure Status
Study Parameters | N | Normal (%) | Pre-Hypertension (%) | Hypertension (%) |
Body Mass Index (kg/m²) | 149 | 90 (12.85%) | 59 (8.42%) | - |
<18.5 (Underweight) | 448 | 238 (34%) | 209 (29.85%) | 1 (0.14%) |
18.5-24.9 (Normal) | 81 | 48 (6.85%) | 33 (4.7%) | 1 (0.14%) |
25.0-29.0 (Overweight) | 22 | 16 (2.2%) | 6 (0.85%) | - |
30.0-34.0 (Obese) | 149 | 90 (12.85%) | 59 (8.42%) | - |
Tobacco Use |
|
|
|
|
No | 659 | 478 (68.2%) | 181 (25.85%) | - |
Yes | 41 | 27 (3.8%) | 12 (1.7%) | 2 (0.28%) |
Alcohol Consumption |
|
|
|
|
No | 526 | 289 (41.2%) | 237 (33.85%) | 2 (0.28%) |
Yes | 174 | 98 (14%) | 76 (10.85%) | - |
Stress Level |
|
|
|
|
Mild | 135 | 71 (10.14%) | 64 (9.14%) | - |
Moderate | 558 | 249 (35.57%) | 309 (44.14%) | - |
Severe | 4 | 2 (0.28%) | 2 (0.28%) | - |
Physical Activity |
|
|
|
|
Active | 324 | 156 (22.28%) | 166 (23.71%) | 2 (0.28%) |
Sedentary | 216 | 100 (14.28%) | 116 (16.67%) | - |
Salt Intake (per day) |
|
|
|
|
>5 g | 340 | 160 (22.8%) | 180 (25.71%) | - |
<5g | 360 | 162 (23.14%) | 196 (28%) | 2 (0.28%) |
Discussion
Table 1 depicts that in present study reported the anthropometric profile of the study population. Mean height, weight (± SD) of the study participants was 166,9±7,6 sm, 59,3±11,2 kg, waist to hip ratio (±SD) of the study participants was 0,9 ±0,002 sm. Mean waist circumferance, hip circumference (±SD) of the study participants was 87,4± 13,3 sm, 94,9± 13,6 sm. Results were similar to Rao et al. [5], who reported that mean height, weight (±SD) of the study participants were 168,3±64,0 sm, 64,5±10,0 kg. Mean waist circumference, waist hip ratio were 77,9±8,1 sm, 0,88±0,10. Results were similar to Midha et al. [6] who reported that mean waist circumference was 78,9±11,0 sm. Nag et al. [7], who reported that mean height, weight (±SD) of the study participants were 115,9±7,8 sm, 67,4±10,5 kg, Mean waist circumference and waist hip ratio were 74,1 ±8.7 sm, 0.9±0.8.
Figure 1 summarizes the blood pressure data and prevalence rates observed in the present study. The mean systolic and diastolic blood pressures were 118.5 ± 8.2 mmHg and 78.5 ± 6.0 mmHg, respectively. The prevalence of normotension, prehypertension, and hypertension was 65 %, 34.85 %, and 0.02 %. These hemodynamic values are consistent with those reported by R. Jayanthi et al. [8] (116.2 ± 13.1 and 74.3 ± 8.7 mmHg) and S. Singh et al. [9] (124.0 ± 15.0 and 83.4 ± 9.5 mmHg). Regarding prevalence, the proportion of prehypertensive individuals in our cohort (34.85 %) aligns with findings from R. Jayanthi et al. [8] (33.85 %) and falls within the range of hypertension/prehypertension rates reported by R. Godara et al. [11] and D.R. Bharati et al. [12] (22.0 and 50.7 %, respectively). In contrast, the prevalence of normotension in our study (65 %) was lower than the 89 % reported by U. Kumar et al. [10], while our hypertension rate (0.02 %) was substantially lower than the rates reported by all cited studies, including U. Kumar et al. [10] (11 %) and R. Jayanthi et al. [8] (5.1 %).
The analysis of risk factors revealed several significant associations. A family history of hypertension was reported in 22.0 % of prehypertensive, 36.7 % of normotensive, and 0.1 % of hypertensive individuals. This distribution differs from the findings of Z. Pilakkadavath et al. [13], who reported a much higher prevalence (76.4 %) among prehypertensive subjects. As summarized in Table 3, the modifiable risk factors analyzed were obesity, physical inactivity, stress, and alcohol and tobacco use. Analysis of dietary salt intake revealed that the prevalence of prehypertension was 28.0 % in subjects consuming more than five grams of salt per day, which was similar than the prevalence of 25.7 % in those consuming less than five grams per day. These finding contrasts with R.B. Singh et al. [14] and C. Bullen et al. [15], who reported that the prevalence of normotension and prehypertension in high salt consumers (> 5 g/day) was 18.1 / 82.0 %, respectively, compared to 22.5 / 84.7 % in low salt consumers. Regarding physical activity, the prevalence of normotension and prehypertension among physically active participants was 22.28 and 23.71 %, respectively. Among sedentary participants, the prevalence was 14.3 % for normotension and 16.7 % for prehypertension. This trend is consistent with R.B. Singh et al. [14] and S. Yadav et al. [16], who reported corresponding rates of 17.9 and 15.3 % in active individuals, and 16.5 and 18.9 % in sedentary individuals. Concerning tobacco use, 3.8 % of tobacco users were normotensive, 1.7 % were prehypertensive, and 0.3 % were hypertensive. These proportions differ from those reported by R.B. Singh et al. [14] and S. Yadav et al. [16], who found that 9.2 % of tobacco users were normotensive, 10.2 % were prehypertensive, and 10.7 % were hypertensive. The overall prevalence of alcohol consumers in our study was 24.9 %, a result similar to the 19.2 % reported by K.R. Thankappan et al. [17]. Furthermore, the prevalence of modifiable risk factors in our population aligns with the broader literature, including R. Ibekwe [18], M.R. Akpa et al. [19], who reported rates forsmoking, alcohol consumption, and obesity of 15.8 %, 43.4 %, and 18.8 %, respectively. Finally, our data on the distribution of risk factors are consistent with V. S. Choudhary et al. [20], who reported that modifiable and non-modifiable risk factors each accounted for 15.3 % of the risk in their study.
Limitations
The age group (18–60 years) predominantly included younger individuals, affecting prevalence estimates. The study was conducted in a single institute and hence results cannot be generalized. Cross-sectional design limits the ability to assess cause-effect relationships.
Conclusion
Pre-hypertensive individuals exhibit a higher prevalence of modifiable risk factors (smoking, alcohol use, physical inactivity, high BMI, central obesity) compared to normotensive individuals. A notable increase in risk factors is observed as individuals’ transition from normotensive to prehypertensive and hypertensive states, suggesting a progressive risk profile. Family history of hypertension, a non-modifiable risk factor, is significantly more common among prehypertensives and hypertensives than normotensives, highlighting the genetic predisposition. Though the number of hypertensive subjects in this study is low, showed multiple associated risk factors, reinforcing the compounded risk from multiple contributors.
References
1. Saseen J. Essential hypertension. In: Alldredge B.K., Corelli R.L., Ernst M.E. et al. Koda-Kimble and Young’s Applied Therapeutics: The Clinical Use of Drugs. 10th ed. Philadelphia: Lippincott Williams & Wilkins;2013;2519.
2. Hypertension Screening, Diagnosis, Assessment, and Managemant of primary Hypertension in adults in India. Ministry of Health & Family Welfare Government of India. 2016;3-143. URL: https://nhm.gov.in/images/pdf/guidelines/nrhm-guidelines/stg/Hypertension_full.pdf?utm_medium=email&utm_source=transaction [accessed: 03.10.2025].
3. World Health Organization, 2013. A Global Brief on Hypertension: Silent Killer, Global Public Health Crisis (WHO, 2013). World Health Organization. Switzerland. URL: https://coilink.org/20.500.12592/stsmc6 [accessed: 03.10.2025]
4. Ahmed N.U., Rahman M., Islam M.D. et al. Socio-demographic clinical characteristics and status of hypertension control among rural hypertensive patient. Faridpur Med. Coll J. 2011;6:5-9. https://doi.org/10.3329/fmcj.v6i1.7402
5. Rao S., Waningankar P. Performance of waist circumference relative to BMI in predicating risk of obesity and hypertension among affluent Indian adults. Health. 2013;(5):16-22. https://doi.org/10.4236/health.2013.58A3003
6. Midha T., Krishna V., Nath B. et al. Cut-off of body mass index and waist circumference to predict hypertension in Indian adults. World J Clin Cases. 2014;2(7):272-278. https://doi.org/10.12998/wjcc.v2.i7.272
7. Karmakar N., Nag K., Saha I. et al. Awareness, treatment, and control of hypertension among adult population in a rural community of Singur block, Hooghly District, West Bengal. J Educ Health Promot. 2018;7:134. https://doi.org/10.4103/jehp.jehp_164_18
8. Jayanthi R., Girijasivam S.P., Nithyavikasini N., Gaur A. Prevalence of prehypertension in young adults in South India. Natl J Physiol Pharm Pharmacol. 2020; 10(11):961-965. https://doi.org/10.5455/njppp.2020.10.07181202013072020
9. Singh S., Shankar R., Singh G.P. Prevalence and Associated Risk Factors of Hypertension: A Cross-Sectional Study in Urban Varanasi. Int J Hypertens. 2017;2017:5491838. https://doi.org/10.1155/2017/5491838
10. Kumar U., Sharma O.P., Goyal J. et al. Prevalence of hypertension among young adults in a Jaipur district of Rajasthan, India. Int J Community Med Public Health. 2017;4:424-7. https://doi.org/10.18203/2394-6040.ijcmph20170266
11. Godara R., Mathews E., Mini G.K., Thankappan K.R. Prevalence, awareness, treatment and control of hypertension among adults aged 30 years and above in Barmer district, Rajasthan, India. Indian Heart J. 2021;73(2):236-238. https://doi.org/10.1016/j.ihj.2021.02.007
12. Bharti D.R., Nandi P., Yamuna T.V. et al. Prevalence and Covariates of Undiagnosed Hypertension in the Adult Population of Puducherry, South India. Nepal Journal of epidemiology. 2012;2(2):191-99. http://dx.doi.org/10.3126/nje.v2i2.6576
13. Pilakkadavath Z., Shaffi M. Modifiable risk factors of hypertension: A hospital-based case-control study from Kerala, India. J Family Med Prim Care. 2016;5(1):114-119. https://doi.org/10.4103/2249-4863.184634.
14. Singh, R.B., Fedacko J., Pella D. et al. Prevalence and risk factors for prehypertension and hypertension in five Indian cities. Acta Cardiologica. 2011;66(1), 29–37. https://doi.org/10.1080/AC.66.1.2064964.
15. Bullen C., Tipene-Leach D., Vander Hoorn S. et al. Ethnic differences in blood pressure: findings from the Fletcher Challenge-Auckland University Heart and Health Study.NZMedJ.1996;109(1032):395-397. URL:https://pubmed.ncbi.nlm.nih.gov/8937388/ [accessed: 03.10.2025].
16. Yadav S., Boddula R., Genitta G. et al. Prevalence & risk factors of pre-hypertension & hypertension in an affluent north Indian population. Indian J Med Res. 2008;128(6):712-720. URL: https://pubmed.ncbi.nlm.nih.gov/19246794/ [accessed: 03.10.2025]
17. Thankappan K.R., Sivasankaran S., Sarma P.S. et al. Prevalence-correlates-awareness-treatment and control of hypertension in kumarakom, kerala: baseline results of a community-based intervention program. Indian Heart J. 2006;58(1):28-33. URL: https://pubmed.ncbi.nlm.nih.gov/18984927/ [accessed: 03.10.2025]
18. Ibekwe R. Modifiable Risk factors of Hypertension and Socio-demographic Profile in Oghara, Delta State; Prevalence and Correlates. Ann Med Health Sci Res. 2015;5(1):71-77. https://doi.org/10.4103/2141-9248.149793
19. Akpa M.R., Emen-chioma P.C., Odia O.J. Current epidemiology of hypertension in port harcount meterpolis Riveres state, Nigeria. Port Harcourt med. J. 2008;2(3):218-223. URL: https://pesquisa.bvsalud.org/portal/resource/pt/afr-192130 [accessed: 03.10.2025]
20. Odia O.J., Emen-chioma Pc. Current epidemiology of hypertension in port harcount meterpolis Riveres state, Nigeria. Port Harcourt med. J. 2008;2:218-23. https://doi.org/10.4314/phmedj.v2i3.38922
21. Virendra S., Choudhary, Devraj Dr. et al. Study of the incidence and risk factors associated with hypertension among adults population residing in Jaipur, Rajasthan. UIJIR.2020;1(1):133-139. URL:https://www.researchgate.net/publication/344557399_STUDY_OF_THE_INCIDENCE_AND_RISK_FACTORS_ASSOCIATED_WITH_HYPERTENSION_AMONG_ADULT_POPULATION_RESIDING_IN_JAIPUR_RAJASTHAN [accessed: 03.10.2025].
About the Authors
Ankita TyagiИндия
MSc Medicine, Department of Physiology, Rajasthan University of Health Sciences, College of Medical Sciences, 302033, Sector-18, Kumbha Marg, Pratap Nagar, Jaipur, Rajasthan, India. ORCID: 0009-0002-7133-5003
Sudhanshu Kacker
Индия
MD, Department of Physiology, Rajasthan University of Health Sciences, College of Medical Sciences, 302033, Sector-18, Kumbha Marg, Pratap Nagar, Jaipur, Rajasthan, India
Neha Saboo
Индия
MD, Department of Physiology, Rajasthan University of Health Sciences, College of Medical Sciences, 302033, Sector-18, Kumbha Marg, Pratap Nagar, Jaipur, Rajasthan, India
Munesh Kumar
Индия
MD, Department of Gastroenterology, Rajasthan University of Health Sciences, College of Medical Sciences, 302033, Sector-18, Kumbha Marg, Pratap Nagar, Jaipur, Rajasthan, India
Supplementary files
Review
For citations:
Tyagi A., Kacker S., Saboo N., Kumar M. PREVALENCE OF CARDIOVASCULAR RISK FACTORS AMONG INDIVIDUALS WITH NORMOTENSION, PREHYPERTENSION, AND HYPERTENSION. Baikal Medical Journal. 2025;4(4):31-38. https://doi.org/10.57256/2949-0715-2025-4-4-31-38
JATS XML
















